At the end of last year, MPs passed an amendment to the National Health Information System Act, making life more difficult for citizens. From the start of the new year, patients are now required to visit their doctors in person for some prescription medications, instead of handling the process electronically.
The amendment, reportedly full of mistakes, proposed by the Health Ministry, was justified as a technical and legislative necessity to comply with European Union regulations on personal data protection related to the electronic prescription service (eRecept). As the Sme daily explains, although the National Health Information Centre manages electronic healthcare, electronic prescriptions are processed by health insurers, which had implemented such systems years before the state. Since January 1, insurers no longer have the “obligation” to process self-payers’ prescriptions to avoid accessing their personal data. As a result, these prescriptions are effectively excluded from the system, making it impossible to upload electronic prescriptions for self-payers.
The law was supported by coalition MPs as well as the opposition party Progressive Slovakia (PS) and was subsequently signed by the president. Now, PS is urging the ministry to expedite changes to address the issue. Back in December, the opposition Christian Democratic Movement (KDH) had already warned that vague wording in the law would make it impossible to issue e-prescriptions for certain medications.
On January 2, the ministry announced an agreement with health insurers and the National Health Information Centre (NCZI) to initiate a legislative process by the end of March to rectify the changes affecting e-prescriptions. Parliament is expected to convene for the first time in early February.
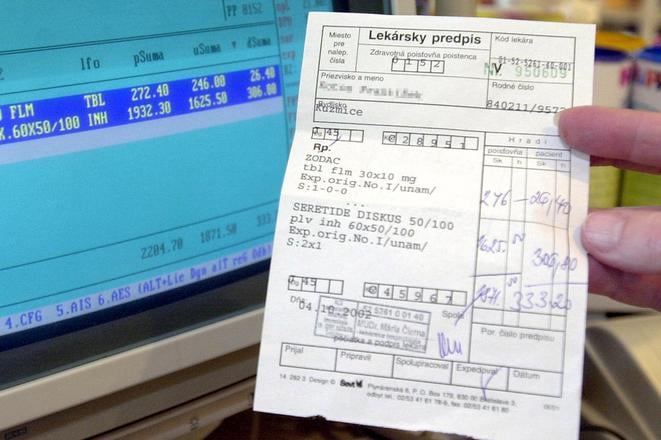
The legislative amendment currently prevents health insurers from processing e-prescriptions for medications, medical aids, and dietary foods not covered by public health insurance and paid for out of pocket. This accounts for nearly a fifth (11-12 million) of all e-prescriptions. Medications such as sleeping pills, sedatives, and vascular treatments must now be prescribed on paper. Other affected prescriptions include medications that patients pay for due to unmet reimbursement criteria, prescriptions from non-contracted doctors (except in urgent care), and medicines imported under special authorisation from the Health Ministry, such as Covid-19 vaccines.
According to Denník N, the controversial change will affect a wide range of medications not covered by health insurance, including eye drops and ointments prescribed for ocular diseases, as well as widely-used drugs such as Ventolin (asthma), Tensiomin (blood pressure), Mydocalm and Sirdalud (muscle relaxation), hormonal contraceptives, and Lexaurin (anxiety). Other impacted treatments include Detralex (venous disease, haemorrhoids), Trifed (cough), Aerinaze (allergies), and optional vaccines. Sme highlighted additional drugs such as Uniflox (antibiotic drops) and Magnosolv.
Paper prescriptions were replaced with electronic ones in 2018.
The Association of Health Insurers has criticised this step back in healthcare digitalisation, warning that it will negatively impact the efficiency of doctors and pharmacies while reducing convenience for patients.
“Electronic prescriptions have significantly reduced overcrowding in waiting rooms and ensured that patients no longer needed to collect prescriptions in person. The system also provides a clearer overview of medications being taken,” said Dajana Petríková, the association’s executive director.
Electronic prescriptions also save time and money for both patients and doctors.